
Police report details grisly crime scene in Greenfield
SUNDERLAND — Police located a cabin in the woods around Clark Mountain Road Thursday afternoon that is believed to belong to Taaniel Herberger-Brown, the suspect accused of murdering a man at 92 Chapman St. in Greenfield and storing his body in a...

Frontier Regional School students appeal to lower voting age
When Sunderland residents head to their Annual Town Meeting on Friday, they’ll vote on the town’s budget, some bylaw changes and a citizen’s petition with a unique twist, as the residents who brought the article forward can’t actually vote on...
Most Read
 Greenfield man arrested in New York on murder charge
Greenfield man arrested in New York on murder charge
 Man allegedly steals $100K worth of items from Northampton, South Deerfield businesses
Man allegedly steals $100K worth of items from Northampton, South Deerfield businesses
 Greenfield Police Logs: April 9 to April 17, 2024
Greenfield Police Logs: April 9 to April 17, 2024
 Former Leyden police chief Daniel Galvis charged with larceny
Former Leyden police chief Daniel Galvis charged with larceny
 Shea Theater mural artist chosen out of 354 applicants
Shea Theater mural artist chosen out of 354 applicants
 Millers Meadow idea would ‘completely transform’ Colrain Street lot in Greenfield
Millers Meadow idea would ‘completely transform’ Colrain Street lot in Greenfield
Editors Picks
 Montague Notebook: April 24, 2024
Montague Notebook: April 24, 2024
 Monroe election sees no contests, some positions without candidates
Monroe election sees no contests, some positions without candidates
 Business Briefs: April 26, 2024
Business Briefs: April 26, 2024
 PHOTO: Spectacular spire
PHOTO: Spectacular spire
Sports

Country Club of Greenfield holding Youth Golf Camp June 24-27
The Country Club of Greenfield is holding its Youth Golf Camp from June 24-27. The camp will be capped at 25 children on a first come, first serve basis. The fee is $170 for the first family member and $140 for each additional family member. The camp...
 High schools: Lilly Ross records 100th career hit in Franklin Tech’s win over Northampton
High schools: Lilly Ross records 100th career hit in Franklin Tech’s win over Northampton
 Baseball: Wyatt Edes’ walk-off single lifts Frontier past Amherst 6-5
Baseball: Wyatt Edes’ walk-off single lifts Frontier past Amherst 6-5
 On The Ridge with Joe Judd: What time should you turkey hunt?
On The Ridge with Joe Judd: What time should you turkey hunt?
 High Schools: Jakhia Williams propels Turners girls track past Athol
High Schools: Jakhia Williams propels Turners girls track past Athol
Opinion

My Turn: A moral justification for civil disobedience to abortion bans
Over the last several years, in response to abortion bans and restrictions, advocates around the country have developed an alternative supply network for abortion pills outside of the medical system and the law.As a lawyer and law-abiding citizen, I...
 Guest columnist Rudy Perkins: Dangerous resolution on Iran
Guest columnist Rudy Perkins: Dangerous resolution on Iran
 Guest columnists Ellen Attaliades and Lynn Ireland: Housing crisis is fueling the human services crisis
Guest columnists Ellen Attaliades and Lynn Ireland: Housing crisis is fueling the human services crisis
 My Turn: April is second chance month
My Turn: April is second chance month

Business

Goddard finds ‘best location’ in Shelburne Falls with new Watermark Gallery space
SHELBURNE FALLS — The 20 Bridge St. space that formerly housed Molly Cantor’s pottery now displays Watermark Gallery’s eclectic collection of modern art pieces.Local artist Laurie Goddard opened Watermark Gallery last month as her seventh location in...
 New buyer of Bernardston’s Windmill Motel looks to resell it, attorney says
New buyer of Bernardston’s Windmill Motel looks to resell it, attorney says
 New owners look to build on Thomas Memorial Golf & Country Club’s strengths
New owners look to build on Thomas Memorial Golf & Country Club’s strengths
 Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
Arts & Life

Sounds Local: A rock circus returns to Turners Falls: The Slambovian Circus of Dreams brings the fun Friday night at the Shea
The circus is coming to town, and not the kind with elephants and clowns. I’m talking about the Slambovian Circus of Dreams, a rock group from the Hudson Valley in New York that makes music as unique as its name. The band, which has frequently...
Obituaries
 Constance Julia Dargis
Constance Julia Dargis
Constance Julia (LaMountain) Dargis Montague Center, MA - Constance "Connie" Julia Dargis, 98, formerly of Turners Falls MA, suffered an unexpected illness on November 13th and passed away peacefully on November 16, 2023 at the home of her ... remainder of obit for Constance Julia Dargis
 John H. Stevens Jr.
John H. Stevens Jr.
John H. Stevens, Jr. Gill, MA - John H. Stevens, Jr., 69, of Main Road died Monday 4/22/24 at home. He was born in Greenfield on December 9, 1954, one of nine children of John H. and Evelyn (Bassett) Stevens. John worked as a papermaker... remainder of obit for John H. Stevens Jr.
 Maryjean DelRosso
Maryjean DelRosso
Heath, MA - Maryjean (Sullivan) DelRosso passed away peacefully on April 19, 2024 at Baystate Medical Center in Springfield after a long illness. She is survived by her devoted husband, Joseph DelRosso. Maryjean is also survived by thr... remainder of obit for Maryjean DelRosso
 Carol Butler Watelet
Carol Butler Watelet
Greenfield, MA - Carol (Virginia) Soucie Butler Watelet, 85, passed away suddenly and peacefully on April 20, 2024, joining the love of her life, Mr. Wonderful, Robert Watelet who passed away 2 years earlier. Carol was born on March 17,... remainder of obit for Carol Butler Watelet

 Montague Cemetery Commission dedicating town’s first green burial site
Montague Cemetery Commission dedicating town’s first green burial site
 Ethics Commission raps former Leyden police chief, captain for conflict of interest violations
Ethics Commission raps former Leyden police chief, captain for conflict of interest violations
 Federal probe targets UMass response to anti-Arab incidents
Federal probe targets UMass response to anti-Arab incidents
 New Salem event will turn gun parts into gardening tools, jewelry
New Salem event will turn gun parts into gardening tools, jewelry
 Advancing water treatment: UMass startup Elateq Inc. wins state grant to deploy new technology
Advancing water treatment: UMass startup Elateq Inc. wins state grant to deploy new technology
 Sunderland Public Library hosting 20th birthday party for its building
Sunderland Public Library hosting 20th birthday party for its building
 Real Estate Transactions: April 26, 2024
Real Estate Transactions: April 26, 2024
 Shelburne fair to explore energy-efficient options for homeowners
Shelburne fair to explore energy-efficient options for homeowners
 Erving rejects trade school’s incomplete proposal for mill reuse
Erving rejects trade school’s incomplete proposal for mill reuse
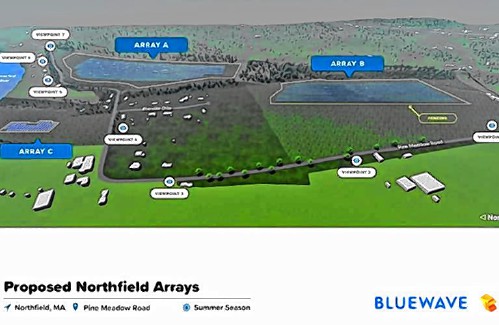 My Turn: Industrial solar installations are overwhelming Northfield neighborhood
My Turn: Industrial solar installations are overwhelming Northfield neighborhood New Realtor Association CEO looks to work collaboratively to maximize housing options
New Realtor Association CEO looks to work collaboratively to maximize housing options Rescuing food and feeding people: Rachel’s Table programs continue to expand throughout western Mass
Rescuing food and feeding people: Rachel’s Table programs continue to expand throughout western Mass A day to commune with nature: Western Mass Herbal Symposium will be held May 11 in Montague
A day to commune with nature: Western Mass Herbal Symposium will be held May 11 in Montague Speaking of Nature: ‘Those sound like chickens’: Wood frogs and spring peepers are back — and loud as ever
Speaking of Nature: ‘Those sound like chickens’: Wood frogs and spring peepers are back — and loud as ever Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28
Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28
