Latest News
 Beacon Hill Roll Call: April 8 to April 12, 2024
Beacon Hill Roll Call: April 8 to April 12, 2024
 My Turn: Saving planet Greenfield
My Turn: Saving planet Greenfield

$50K allocated for Poet’s Seat Tower sandblasting as officials mull vandalism prevention
GREENFIELD — Following an affirmative vote by City Council this week, $50,000 will go toward sandblasting graffiti off of Poet’s Seat Tower, where vandalism has proven to be a persistent problem.Department of Public Works Director Marlo Warner II said...

PHOTOS: Convening for a good cause
Most Read
 New owners look to build on Thomas Memorial Golf & Country Club’s strengths
New owners look to build on Thomas Memorial Golf & Country Club’s strengths
 Orange man gets 12 to 14 years for child rape
Orange man gets 12 to 14 years for child rape
 Greenfield Police Logs: April 2 to April 8, 2024
Greenfield Police Logs: April 2 to April 8, 2024
 One Greenfield home invasion defendant up for bail, other three held
One Greenfield home invasion defendant up for bail, other three held
 Fire scorches garage on Homestead Avenue in Greenfield
Fire scorches garage on Homestead Avenue in Greenfield
 Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
Editors Picks
 Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
 PHOTO: Double eagle
PHOTO: Double eagle
 North County Notebook: April 20, 2024
North County Notebook: April 20, 2024
 Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear
Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear
Sports

High schools: South Hadley softball holds off Frontier rally for 5-4 victory (PHOTOS)
A day after completing a comeback victory over Greenfield, the Frontier softball team looked like it had another rally in the works on Friday against South Hadley.The Tigers held a 1-0 lead going into the sixth inning when the Redhawks rallied,...
Opinion

Jessica Zhang: Weigh your choices — Solar power a better alternative
In his recent letter [“‘No’ means higher energy prices,” Recorder, March 26] Jim Bates is right that fossil fuels have powered societies across the globe — nobody disputes that. It’s the reality of pollution and carbon buildup in the atmosphere that...
 Gary Seldon: Solar Roller Earth Day River Ride
Gary Seldon: Solar Roller Earth Day River Ride
 Columnist Johanna Neumann: Reaping the rewards of rooftop solar
Columnist Johanna Neumann: Reaping the rewards of rooftop solar
 My Turn: Let’s leave miracle of trees well enough alone
My Turn: Let’s leave miracle of trees well enough alone

Business

New owners look to build on Thomas Memorial Golf & Country Club’s strengths
TURNERS FALLS — Members of the Snow family have added another golf course to their portfolio and have already begun work on cosmetic improvements.Kyle and Kelly Snow, along with Kyle’s parents Edward Snow Jr. and Kerrilynn Snow, bought the Thomas...
 Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
 Tea Guys of Whately owes $2M for breach of contract, judge rules
Tea Guys of Whately owes $2M for breach of contract, judge rules
 Primo Restaurant & Pizzeria in South Deerfield under new ownership
Primo Restaurant & Pizzeria in South Deerfield under new ownership
 Patrons can ‘walk down memory lane’ at Sweet Phoenix’s new Greenfield location
Patrons can ‘walk down memory lane’ at Sweet Phoenix’s new Greenfield location
Arts & Life

Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28
A lot can change in 20 years: Presidents and other politicians come and go, new cultural fads and technologies emerge, clothing styles morph, and music and movies take on different dimensions.In these parts, one tradition hasn’t changed. Since 2005,...
Obituaries
 Judith Fuhring Seelig
Judith Fuhring Seelig
Amherst, MA - Judith (Fuhring) Seelig passed away peacefully at Cooley Dickinson Hospital on October 21, 2023 after a brief illness. She was surrounded by friends and family with music and ... remainder of obit for Judith Fuhring Seelig
 Richard F. Delphia
Richard F. Delphia
Ashfield, MA - Richard F. Delphia, 84, passed away at Baystate Medical Center in Springfield on Tuesday, April 16, 2024, of complications from a fall. Dick was born in Ludlow, MA on Aug... remainder of obit for Richard F. Delphia
 Mary Lou Barton
Mary Lou Barton
Leyden, MA - Mary Lou (Johnson) Barton, 74, of Leyden MA, took the Lord's hand on April 16, 2024, surrounded by her loving family at home. She was born in Brattleboro, VT on September 7, 19... remainder of obit for Mary Lou Barton
 Judith M. Lively
Judith M. Lively
Greenfield, MA - Judith Mae (Phillips) Lively, 85, of Wells St., passed away on Tuesday April 9, 2024. Judy was born in Greenfield on June 5, 1938 the daughter of Walter and Mildred (Ch... remainder of obit for Judith M. Lively

 Connecting the Dots: In what world do you want to live?
Connecting the Dots: In what world do you want to live?
 ‘Glamping’ resort developers look to curb traffic, sewer concerns in Charlemont
‘Glamping’ resort developers look to curb traffic, sewer concerns in Charlemont
 As emergency action plan is crafted, Tree House to maintain 1,500 capacity for summer
As emergency action plan is crafted, Tree House to maintain 1,500 capacity for summer
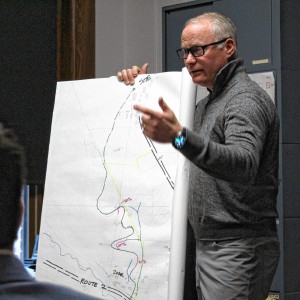
 MassDOT shares plans for Church Street bridge replacement in Erving
MassDOT shares plans for Church Street bridge replacement in Erving
 Proposed Colrain solar bylaw changes would add definitions, expand site plan reviews
Proposed Colrain solar bylaw changes would add definitions, expand site plan reviews
 Deerfield voters to decide 8 capital projects at Town Meeting
Deerfield voters to decide 8 capital projects at Town Meeting
 Shelter money fading, but ‘not at the end of the line’
Shelter money fading, but ‘not at the end of the line’
 Softball: Franklin Tech’s Hannah Gilbert holds Hopkins to two hits, leads Eagles to 7-1 victory (PHOTOS)
Softball: Franklin Tech’s Hannah Gilbert holds Hopkins to two hits, leads Eagles to 7-1 victory (PHOTOS) Keeping Score with Chip Ainsworth: What’s ahead for Greg Carvel’s crew?
Keeping Score with Chip Ainsworth: What’s ahead for Greg Carvel’s crew? High schools: Abigail Schreiber’s hit propels Frontier softball past Greenfield, 3-2
High schools: Abigail Schreiber’s hit propels Frontier softball past Greenfield, 3-2 Baseball: Frontier handles Greenfield 12-2 in five-inning victory (PHOTOS)
Baseball: Frontier handles Greenfield 12-2 in five-inning victory (PHOTOS) Mitch Speight and Joan Marie Jackson: City should follow constitutional ruling on property takings
Mitch Speight and Joan Marie Jackson: City should follow constitutional ruling on property takings Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many
Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many Earth Matters: From Big Sits to Birdathons: Birding competitions far and near
Earth Matters: From Big Sits to Birdathons: Birding competitions far and near Sounds Local: Spring is singer-songwriter season: A host of local performers celebrate new work
Sounds Local: Spring is singer-songwriter season: A host of local performers celebrate new work Crunch time for matzo: An easy-to-make sweet treat that’s Passover Seder-friendly
Crunch time for matzo: An easy-to-make sweet treat that’s Passover Seder-friendly
