
Millers Meadow idea would ‘completely transform’ Colrain Street lot in Greenfield
GREENFIELD — The environmental nonprofit Greening Greenfield is seeking the city’s approval to plant a small forest and meadow along the perimeter of the former site of the Wedgewood Gardens mobile home park on Colrain Street.If approved, the group...

Greenfield’s Court Square to remain open year-round for first time since 2021
GREENFIELD — For the first time since 2021, Court Square will stay open to motorists year-round, closing only for special events that require pedestrian access.The city began seasonally closing Court Square to vehicles in 2021 when it adopted a pilot...
Most Read
 Former Leyden police chief Daniel Galvis charged with larceny
Former Leyden police chief Daniel Galvis charged with larceny
 My Turn: The truth about time spent on MCAS testing
My Turn: The truth about time spent on MCAS testing
 GMLB, Newt Guilbault gets seasons underway Sunday (PHOTOS)
GMLB, Newt Guilbault gets seasons underway Sunday (PHOTOS)
 Millers Meadow idea would ‘completely transform’ Colrain Street lot in Greenfield
Millers Meadow idea would ‘completely transform’ Colrain Street lot in Greenfield
 Bulletin Board: Gary Tashjian, Cheri McCarthy win Twice As Smart Pickleball Tournament
Bulletin Board: Gary Tashjian, Cheri McCarthy win Twice As Smart Pickleball Tournament
 Greenfield Girls Softball League opens its 2024 season (PHOTOS)
Greenfield Girls Softball League opens its 2024 season (PHOTOS)
Editors Picks
 PHOTOS: Artsy and informative
PHOTOS: Artsy and informative
 Greenfield High School Honor Roll, Third Quarter
Greenfield High School Honor Roll, Third Quarter
 West County Notebook: April 23, 2024
West County Notebook: April 23, 2024
 Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear
Best Bites: A familiar feast: The Passover Seder traditions and tastes my family holds dear
Sports

High schools: Skyler Steele powers Frontier softball past Wahconah
It was a birthday to remember for Skyler Steele.The Frontier slugger smacked a home run and drove in five runs as the Redhawks cruised to a 15-3 victory over Wahconah in a Franklin County League West contest on Monday at Zabek Field in South...
 Bulletin board: Landon Allenby, Lucas Allenby shine at USA Snowboard and Freeski Association Nationals
Bulletin board: Landon Allenby, Lucas Allenby shine at USA Snowboard and Freeski Association Nationals
 Baseball: Athol outlasts Franklin Tech in nine-inning thriller (PHOTOS)
Baseball: Athol outlasts Franklin Tech in nine-inning thriller (PHOTOS)
 GMLB, Newt Guilbault gets seasons underway Sunday (PHOTOS)
GMLB, Newt Guilbault gets seasons underway Sunday (PHOTOS)
Opinion

My Turn: National debt — A threat to our nation’s future
This is an update on a column I wrote last year about a threat to our future well-being: the national debt. To summarize, unless the debt crisis is brought under control soon the future will be much more difficult for you, your children, grandchildren...
 Josie Silva: Voting age impacts voter turnout
Josie Silva: Voting age impacts voter turnout
 Ferd Wulkan: Green schools are possible
Ferd Wulkan: Green schools are possible
 Jessica Corwin: Lower voting age to strengthen democracy
Jessica Corwin: Lower voting age to strengthen democracy
 Erika Heilig: Trump’s mug is not news
Erika Heilig: Trump’s mug is not news

Business

New Realtor Association CEO looks to work collaboratively to maximize housing options
SPRINGFIELD — As the Realtor Association of Pioneer Valley’s new CEO arrives to a Massachusetts housing market plagued by high prices and a lack of stock, he aims to work alongside elected officials to maximize the availability of different kinds of...
 New owners look to build on Thomas Memorial Golf & Country Club’s strengths
New owners look to build on Thomas Memorial Golf & Country Club’s strengths
 Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
Cleary Jewelers plans to retain shop at former Wilson’s building until 2029
 Tea Guys of Whately owes $2M for breach of contract, judge rules
Tea Guys of Whately owes $2M for breach of contract, judge rules
 Primo Restaurant & Pizzeria in South Deerfield under new ownership
Primo Restaurant & Pizzeria in South Deerfield under new ownership
Arts & Life

A day to commune with nature: Western Mass Herbal Symposium will be held May 11 in Montague
This week’s feature is my 100th Home & Garden column for the Recorder, and I’m pleased to celebrate by sharing the plans of two local women who are organizing a remarkable event for anyone interested in learning about herbal remedies and natural...
Obituaries
 Raymond E. Scott
Raymond E. Scott
Raymond E. "Ray" Scott Bunnell, FL - Raymond E. "Ray" Scott, 78, of Bunnell, Florida passed away August 15, 2023. Ray was born in Yonkers, NY March 19, 1945. He was the son of Allan and Selva (Barney) Scott. Ray moved to Buckland as a yo... remainder of obit for Raymond E. Scott
 John Kubacki Jr.
John Kubacki Jr.
John Kubacki, Jr. Palm Bay, FL - John Kubacki, Jr., 75 years old, of Palm Bay, Florida died peacefully on Wednesday, April 17, 2024 surrounded by his loving family. He was born on October 8, 1948, the son of Irene and John Kubacki Sr. ... remainder of obit for John Kubacki Jr.
 Frank Kelley
Frank Kelley
Keene, NH - Frank S. Kelley, 93 of Keene, N.H. formerly of Greenfield, Mass and Northfield, Mass. died Thursday (4-18-2024) at Cheshire Medical Center, Keene, N.H. He was born in Orange, Ma. on February 23, 1931, the son of Burton and M... remainder of obit for Frank Kelley
 Diane H. Overstreet
Diane H. Overstreet
Greenfield, MA - Diane H. Overstreet (Glazier) of Greenfield succumbed to a short battle with cancer on Wednesday March 27th, 2024, at the age of 75. Born June 2nd, 1948, in Greenfield, Massachusetts to Warren and Bernice Glazier. D... remainder of obit for Diane H. Overstreet

 Prescription drug take back day set for Saturday in 15 communities in Franklin, Hampshire counties
Prescription drug take back day set for Saturday in 15 communities in Franklin, Hampshire counties
 Leverett Town Meeting voters will decide cease-fire call, budgets
Leverett Town Meeting voters will decide cease-fire call, budgets
 Judge dismisses case against former Buckland police chief
Judge dismisses case against former Buckland police chief
 $10K grant to build on Erving Public Library’s work with neurodivergent patrons
$10K grant to build on Erving Public Library’s work with neurodivergent patrons
 Greenfield Police Logs: April 9 to April 17, 2024
Greenfield Police Logs: April 9 to April 17, 2024
 Dual fundraisers in Bernardston to support The United Arc, Sgt. Jacob Garmalo Fund
Dual fundraisers in Bernardston to support The United Arc, Sgt. Jacob Garmalo Fund
 Glass, sculpture artists to be featured at Salmon Falls Gallery
Glass, sculpture artists to be featured at Salmon Falls Gallery
 Greenfield lifts cap on cannabis delivery operators as CCC guidelines expand access
Greenfield lifts cap on cannabis delivery operators as CCC guidelines expand access
 Bulletin Board: Gary Tashjian, Cheri McCarthy win Twice As Smart Pickleball Tournament
Bulletin Board: Gary Tashjian, Cheri McCarthy win Twice As Smart Pickleball Tournament Speaking of Nature: ‘Those sound like chickens’: Wood frogs and spring peepers are back — and loud as ever
Speaking of Nature: ‘Those sound like chickens’: Wood frogs and spring peepers are back — and loud as ever Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28
Hitting the ceramic circuit: Asparagus Valley Pottery Trail turns 20 years old, April 27-28 Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many
Valley Bounty: Your soil will thank you: As garden season gets underway, Whately farm provides ‘black gold’ to many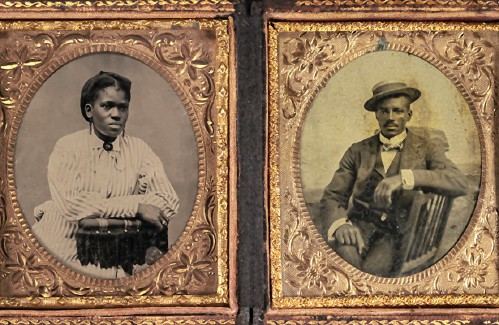 Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
Painting a more complete picture: ‘Unnamed Figures’ highlights Black presence and absence in early American history
